Integrated health and social care - an ICS prototype case study
Creating a person centred ICS in a locality, redesign of NHS and social care services, using a strengths based systems thinking method
The Setup of the ICS |
The Problem to SolveTaking care of people, their health and welfare needs, their social issues, and their relationships. This has to be one of the most complex systems that anyone can work in. Especially as this has to include the community and family circumstances, as well as the individual.
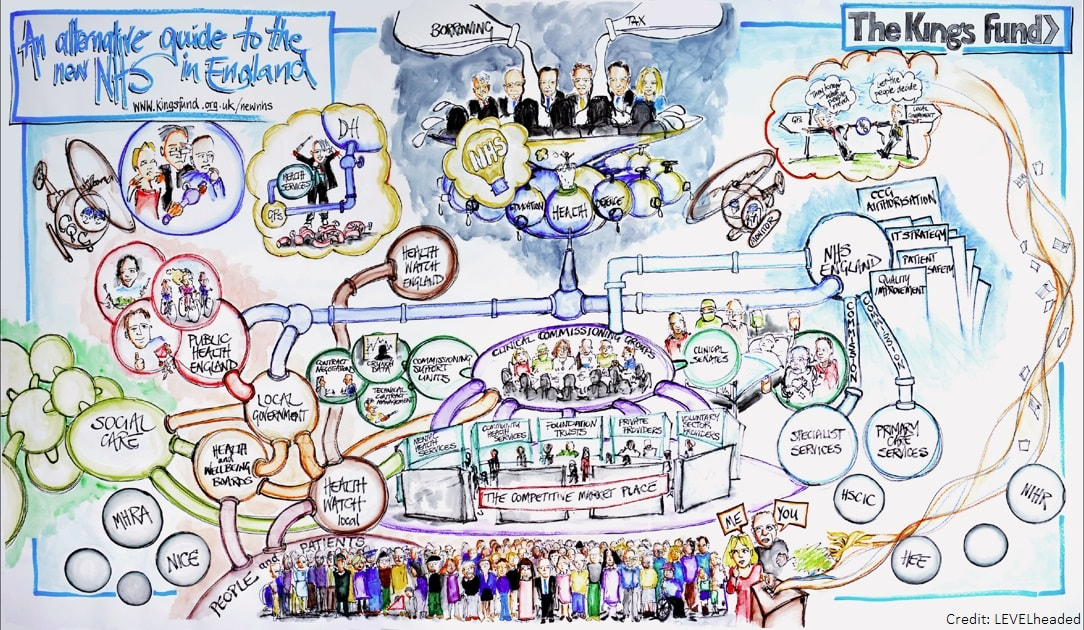
In England we have made it particularly complex, by the way government has seen fit to design the overall health and social care system. By fragmenting the various 'services' and privatise provision, this has unleashed forces that guide the behaviour of a miriad of organisations with different competencies and rules. A systems approach is particularly apt to make sense of this complexity. It strips out the artificial barriers that are put in the way of doing the right thing, and allows a design of an effective system to emerge. Many authorities are now experimenting with integrated and strength based working. The government and the NHS have recognised that the way forward is more integrated care. Integrated working ICS developing by each trust are now focusing on transformation and localisation of care. Personalisation, patient centered, community, integration, strength based, key worker... They are all pushing against the monolithic approach of treating everyone the same. Now that this approach has proven itself, lets get going with what we have learned works. Increasing demand into the health system, and signs of increasing waste in processes has been a factor in public healthcare for a number of years now. In particular, there has been a recent awareness amongst managers that the service that was being delivered is not a good service. The PlanThe task is to create an example of what is possible if the system is completely redesigned from a different perspective; eliminating the major barriers to effective working.
A full-time team was put together of all the disciplines required to deal with citizens who have community health needs. The team included an operational as well as a senior manager, and the team had direct links with the hospital, GPs and specialist health services. |
The service as it was |
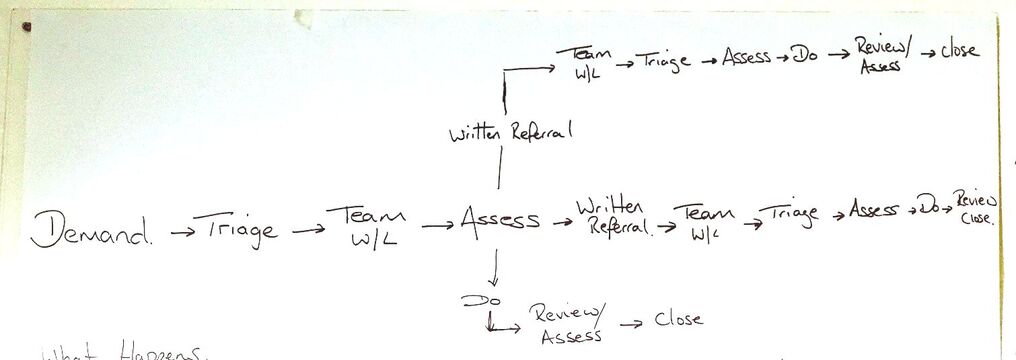
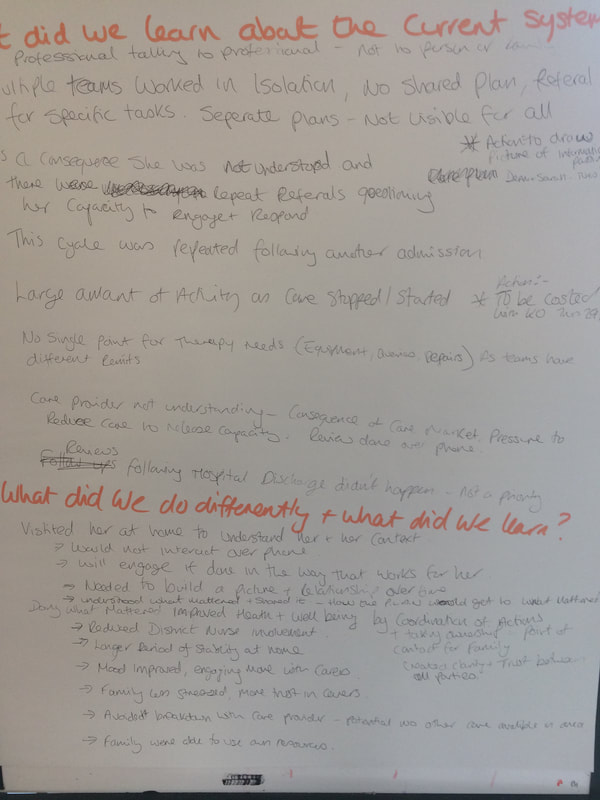
What was foundThe team found that the current system was very inefficient and ineffective. This was characterised by high levels of waste in the operations. But more importantly, the citizen was being taken through a series of rule driven complicated steps, that that did not contribute to dealing effectively with the persons problems.
The managers realised that they were partially responsible for this current situation as they had put in a series of assessments and rules that were designed to help staff to follow a standard process, to reduce risk, and to minimise cost. Those in the work were bombarded with increasing levels of demands on their time, creating a highly stressful and activity focused mindset, resulting in low morale and a personal distancing from what really mattered to patients.
It was realised that citizens core issues were often not resolved until too late if at all, resulting in months or years of unnecessary treatments. Citizens would bounce around the public health system with little progress of improvement to their overall lives. |
The Experiment - liberating method |
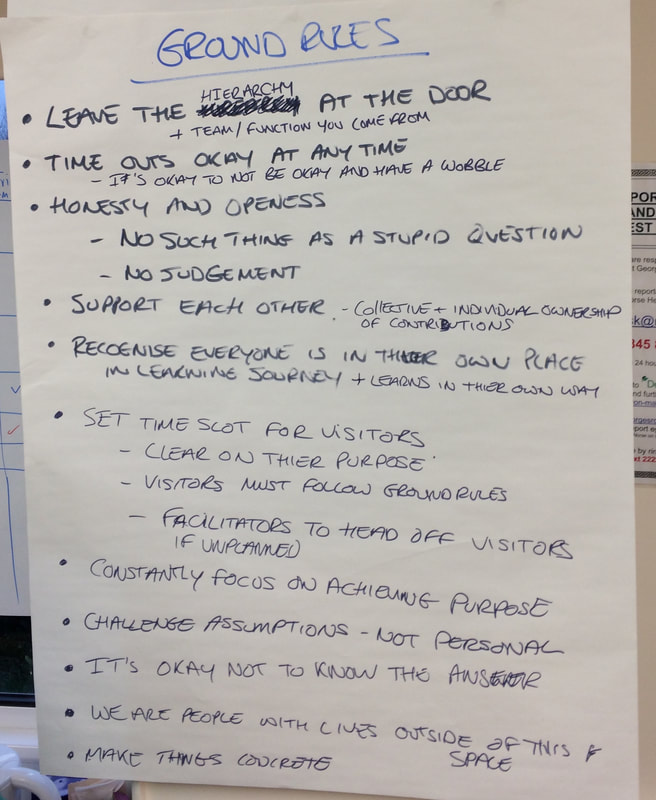
Applying a systems thinking perspective to this problemAn important part of the intervention design methodology, is a safe to try environment. The team were given a physical room, so they could be disconnected with the current mindset, procedures, culture and ways of working of the current organisation. I call this 'the bubble' which is an innovation method that is designed to allow for people to truly come up with new ways of working unencumbered by the current systemic conditions. The team are led to work as a cross-functional design team, across their specialisms, on the end to end service, to focus on learning by taking customer demands directly into the team.
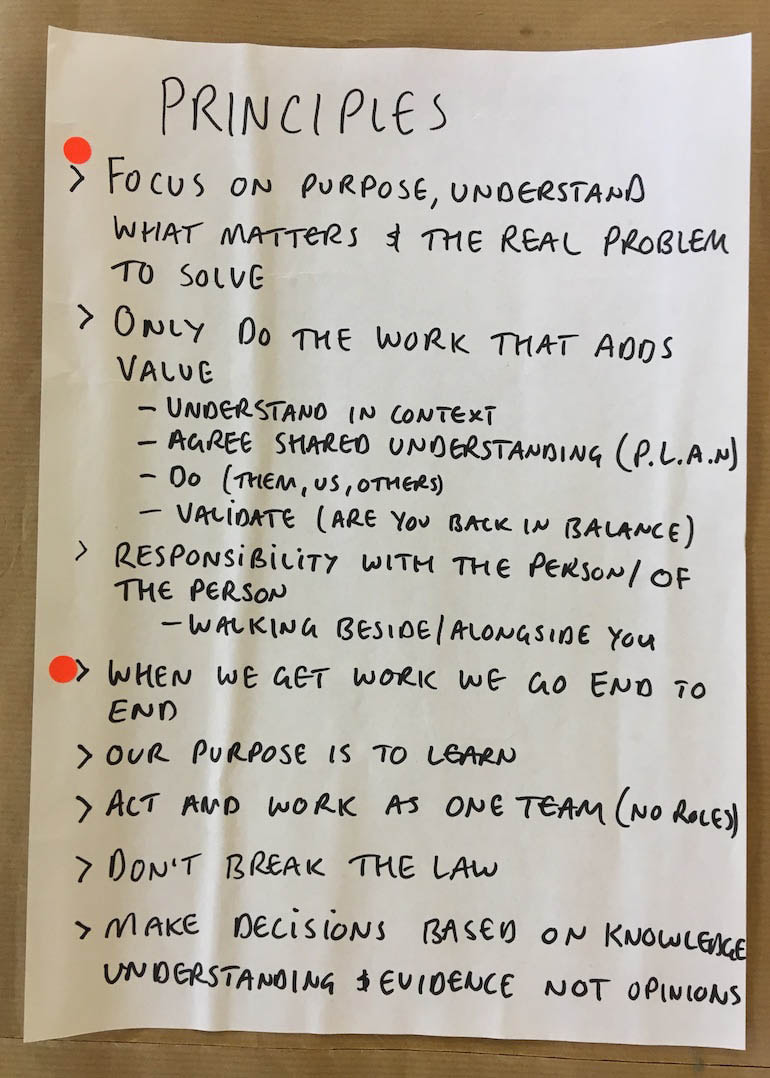
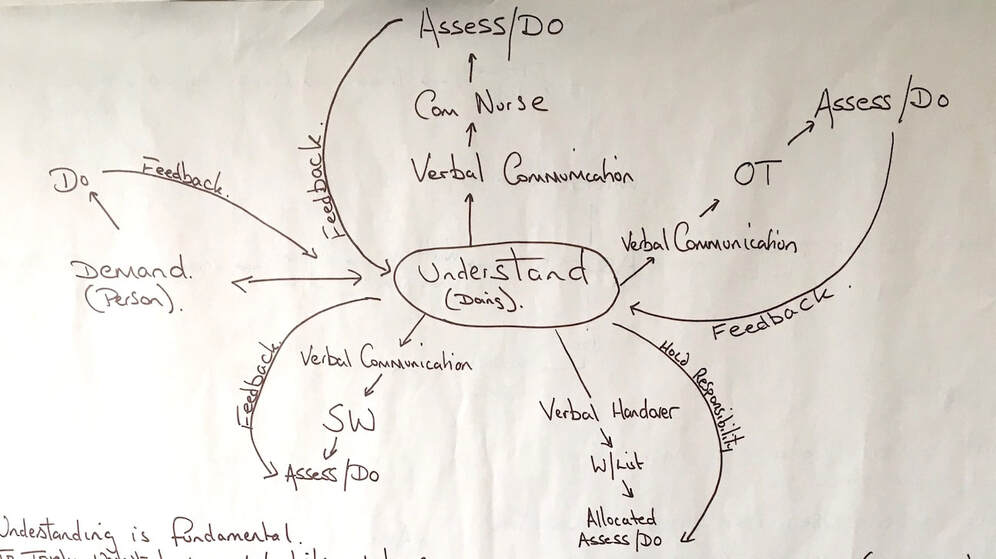
We started with a new perspective, principles based on 'the liberated method' working in local government with people who need us:- Understand what matters for each person, this determines the design. - We make decisions based on knowledge and evidence, not opinion or standards. - Only do what is needed to create value, enabling the person to gain control. - Take ownership through the end to end journey with the person. - Work as a team, without department barriers. - We are here to learn, and improve. Rule 1 - do not break the law. Rule 2 - do not make their situation worse. The team picked randomly, real demands, and began to deal with them from end to end - start to finish as defined by the person. They started by focusing on the needs of the citizen by applying a set of new operating principles to each person (pic below). This liberated the staff from the old methods of working, and gave them a framework to move forward in a specific direction to focus on delivering value. This strength based approach allowed the team to learn how to approach and deal with people in a way that focused on getting them back to a stable and healthy state, and not simply reacting to what was written on the referral sheet! To enable this experimentation, the barriers to making this happen had to be temporarily suspended by the leadership, including any time or other restrictions that would normally be in place. The staff were so conditioned by rules, that the team were surprised at how difficult it was to learn how to actually listen and understand someone's life context free of pre-determined structures. It took over a week of working together, to wean themselves off using standard assessments. |
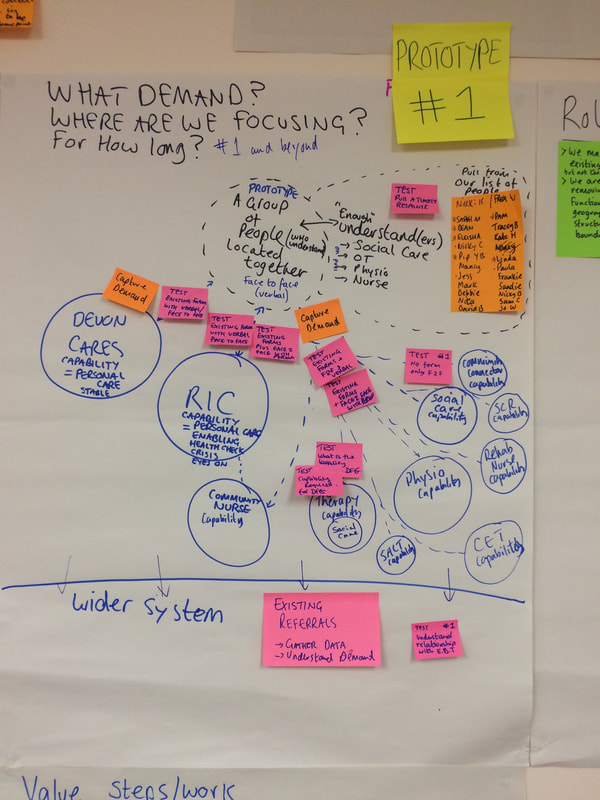
The systemic prototype |
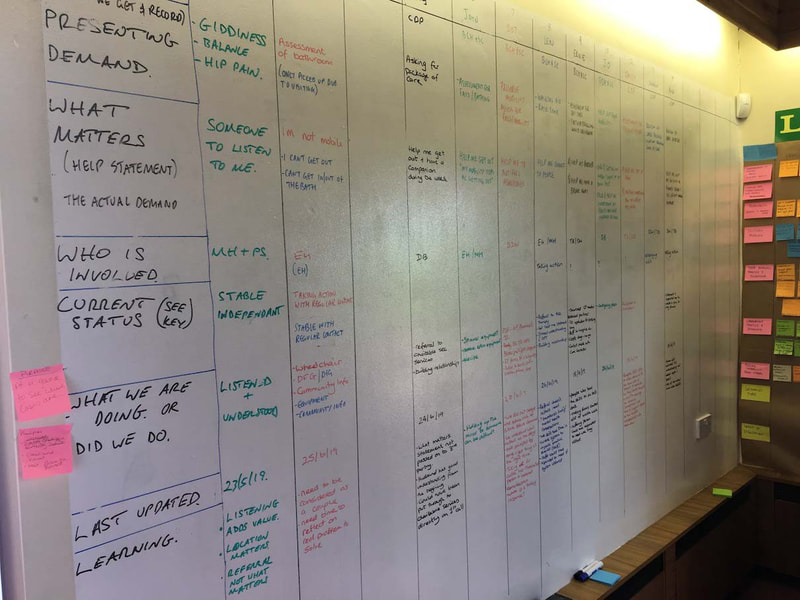
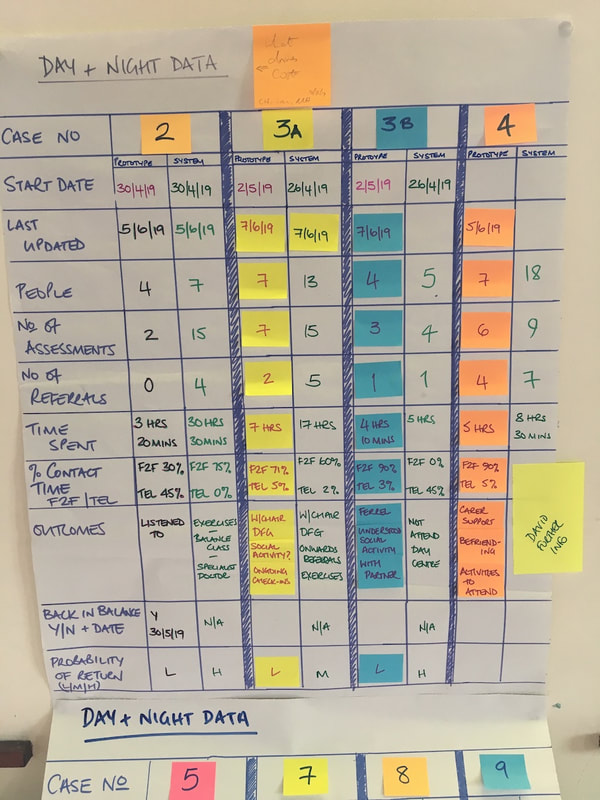
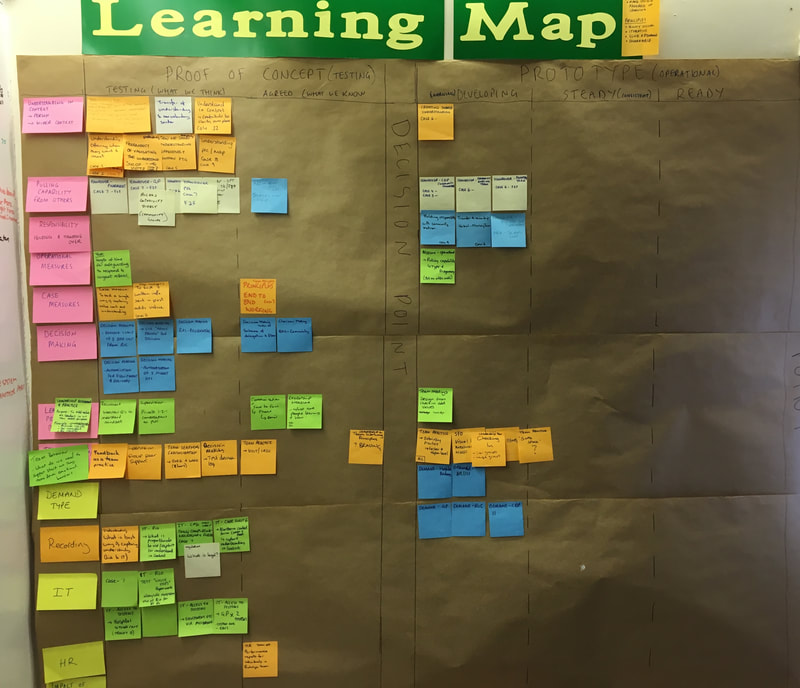
After several months, after the team had taken 35 people through the new principles. Over this time, they measured the outcomes of their experiments. A new way forward began to emerge of both the process that we could take people through and how we might work together as a team and with our managers. Importantly for the managers and leaders, we also discovered what elements in the existing system has to change to enable this new way of working to be supported and allowed to operate successfully.
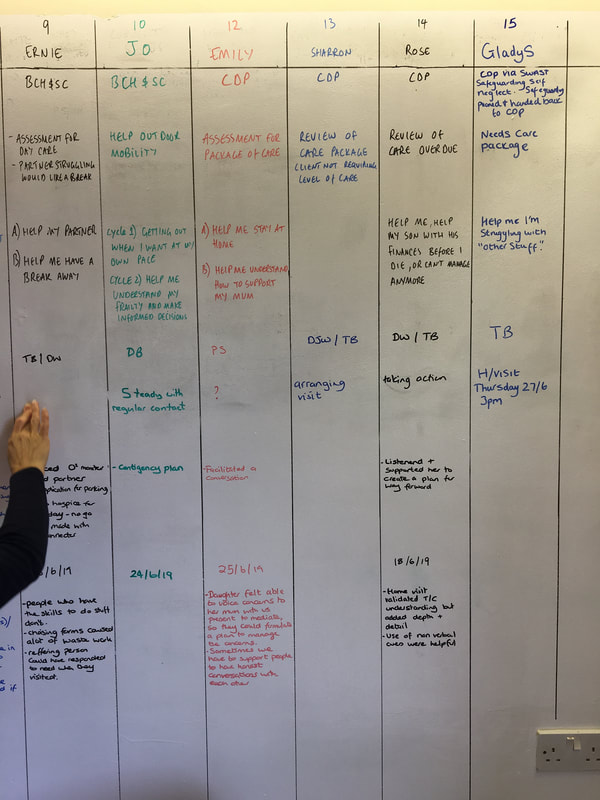
Step 1 Understand me & what matters to meEach team member took demands, and the first step was always to understand the nature of why the person had come to them in the first place. In most cases this required a visit. Listening and learning about their issues, and whatever they wanted to tell us. We discovered that this was often about life issues, living situations, relationship problems. That activity continued until they developed a level of trust and got to learn clearly what mattered to that person.
Understand each person in their environment and those around them. Step 2 Decide the best agreed course of actionLiberating the front line from their old methods, using a new set of principles. This is about assessing the whole situation of the person, their environment, and their friends and family. In the majority of cases what was required had little to do with clinical help. There were few restrictions placed on the team, and they were able to pull on any of the clinical expertise from anyone in their team if needed.
Step 3 Keep ownership, and maintain the person to get back into balance We are engaging with them and are directly available at the end of the phone if required. Whatever the team think needs recording is written down. This is where we don't simply close the case, we ensure that they have got to a place of stability.
Step 4 CloseWe close the case when we have agreed with them that we have provided enough support. If they contact us again, the same team member is assigned the case again.
|
The new design detail
After the completion of the experiment, the team with the manager and leaders prepared for the prototype to start. For this to occur, the concepts and methods had to be formulated and designed to a level of operational detail. A new process and new measures emerged, and the element below are the main aspect do the prototype.
Purpose & the Relationship with Citizens
The actual purpose of the service that the managers focus on, then drives that which the staff focus on. In the NHS currently this purpose is an internally driven focus based on cost and a raft of measures. This real purpose of a service is often never discussed or understood openly. But we did discuss it, and we came up with our strengths based purpose.
|
Old purpose
'What is the matter with you', and then to work on the task infront of me, as quickly as possible, following all the rules.
It drives me to lose sight of actually helping someone, and I feel relieved when I can refer it on to someone else.
|
New Person centred purpose
' What matters to you', and how can I help the person to achieve balance in their lives.
It drives me to focus on what matters, and to only do those value activities that I need to.
|
As we were examining the service from a citizen perspective, the relationship we have with them changed...
Relationship with citizens moves from; engage with us (on our terms), to engage with you (what suits you).
Power moves from; power over others, to power with.
These are two fundamental changes to the way that we perceive how our service interacts with citizens. We began to understand what putting the citizen in the centre of the design really was about.
Relationship with citizens moves from; engage with us (on our terms), to engage with you (what suits you).
Power moves from; power over others, to power with.
These are two fundamental changes to the way that we perceive how our service interacts with citizens. We began to understand what putting the citizen in the centre of the design really was about.
And if the services are redesigned around this new purpose, what do you think will happen? Will delivering a personalised service cost more? That is one answer that we found below.
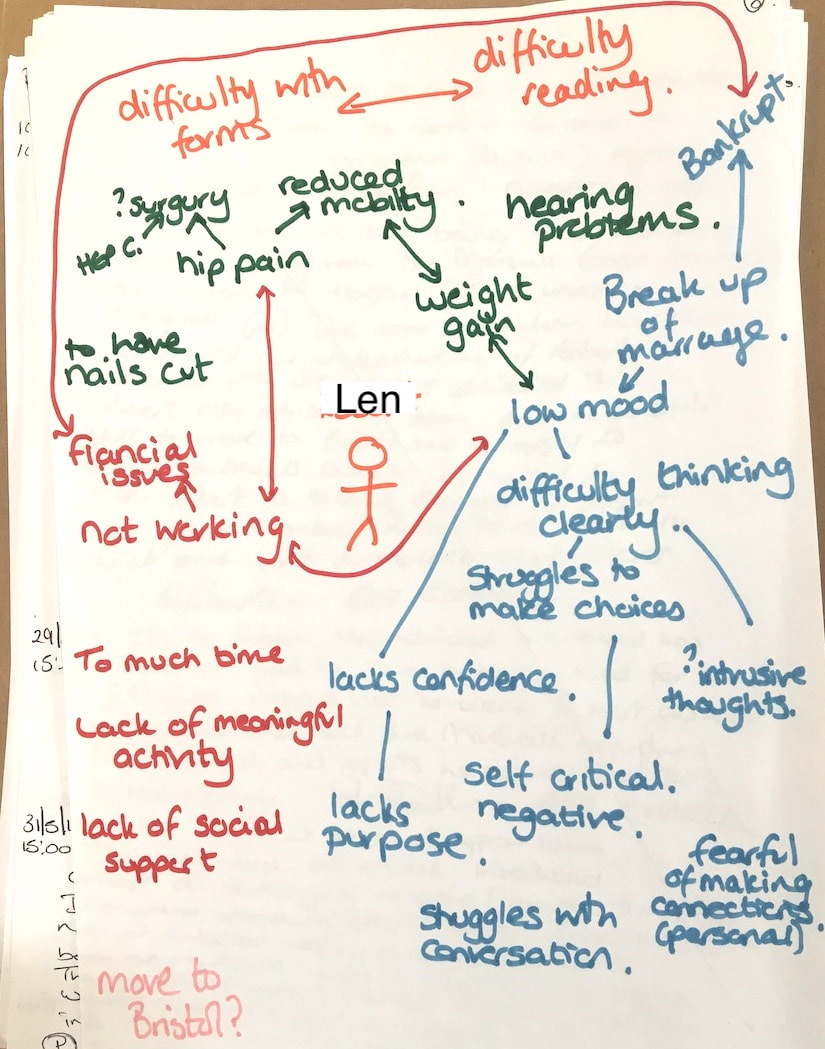
Len, a case study as presented to the senior leaders
The power of story-telling, to describe a complex situation. If you want to experience what this is actually like to be taken through a strength based prototype by the team, and you have about 16 minutes, you can experience it below, Eleisha talking about Len. Senior managers of the ICS were in the audience.
Health and Social Care strength based Integrated Care System prototype. Len's Story.
Outcomes |
As an example, this is what we found about one of the people, Anne
My problem – I have complications with my wrists, and everything I touch feels hot. It is a condition that is not curable. What matters to me - I need help to live as normal life as much as possible. I need help dressing, cleaning the house and cooking.
The solution was not about fixing her chronic condition, it was actually about helping her to continue to live her life as normal as possible. What we provided was adaptations and advice. We also found a teenager who lived neardy that needed help with her reading and writing, which Anne was very happy to help with, in exchange for the teen helping around the house with cleaning. Before we took this case on, Anne had been bouncing around the service with five referrals that had no meaningful impact over two years. This was a typical case that would bounce round the community health office, and over time the service user would either make repeated demands, or lose interest and stop connecting with the health service. A typical failed outcome that shows how we can spend lots of time going round in circles.
It's tempting to view this experiment work as simply introducing a 'single point of contact', or a 'multi-disciplinary hub', or 'sharing data'. The reality is that the real change is in the thinking and approaches of those in the new system, in Anne's case above, one person actually did most of the value work with a new decision framework and the ability to make local decisions. It took senior managers to give the team permission to avoid what we needed to liberate method:
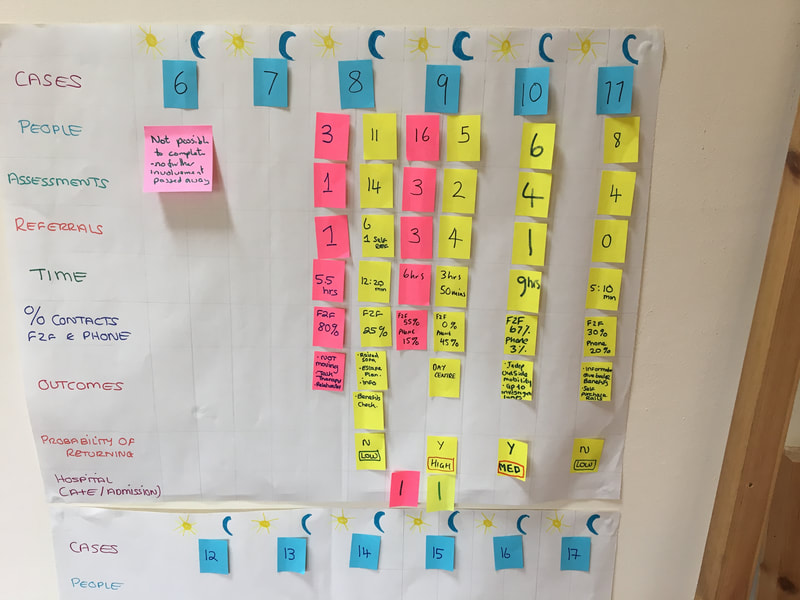
MeasuresThe summary of all the 35 people we worked with in the experiment
66% of the demand originally recorded on the system, did not match the real problem to solve. All the demands taken were complex, highlighting the fact that by liberating front line workers to adopt a flexible and non-standard design of the work was appropriate. This is in contrast to a non-complex demand like; I have sprained my ankle (with no associated issues).
By getting good understanding, and work with the cases end to end, we reduced repeat demands into the service from 71% to almost 0%. If you would like to see more about the measures and how the team developed them
Leadership and management
The effect on the teamThe team developed a new way of working together, that allowed them to be open and honest with each other.
This is a team member, an Occupational Therapist, explaining how her behaviour in the current design was driving her behaviour in the wrong way (1 min)
|
What happened to this work? The mean and leaders had agreed to take the prototype and make it work in a locality. Then Covid struck... And thats it.
The learning
|
In this health system, services like this develop such waste and poor outcomes due to the functional mechanistic and controlled nature and standardisation of the flow of work. The learning from a managers perspective was that if they truly looked at their service end to end, and that by understanding the real demand and what matters to people should drive the work that we need to do. Strength based. So, unless the systemic problems were redesigned, no amount of changing of rules, procedures, or IT system results in real sustained improvement
|
Delivering care across existing systems will be a key development for the future of service delivery and evidence suggests that a “systems thinking approach” will be required to understand the environment and the complex interactions within it.
Commissioning for Effective Service Transformation, NHS England
Systemic Design workshop
Find this interesting? How about joining a systemic design masterclass to learn how to apply this
Practical steps you can take
From working with various ICS's and various service redesigns, we have learned a few practical activities and areas to focus on that make a significant impact on a health service. Use the button below to go to that list of practical steps.
Webinar of the ICS prototype
Here is a webinar with John Mortimer and member of the team, that describes this whole case study
Delving deeper into the methodology; Design thinking, Service design and Systems thinking
You can read another case study, about Bob whom we learned lots about how to do things right
If you want to know more about the detail of the design and systems thinking methodology used, it is described in this section...
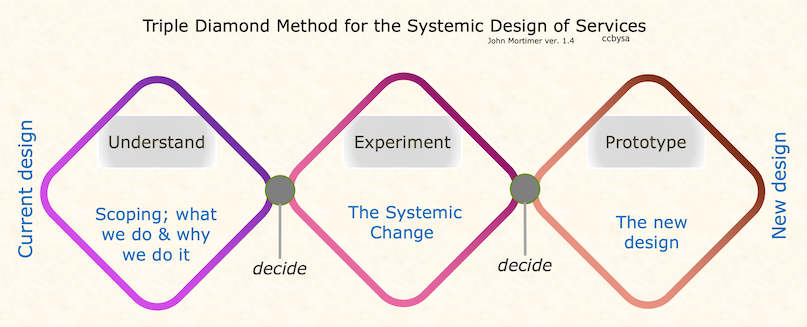
The approach that this piece of work took combined Design Thinking principles with Systemic Design and System Thinking. Each 'thinking' is woven into the overall methodology, so that in one morning, the conversations will always start with what matters to the end user, and incorporate an end to end perspective. We challenged everything, liberating the method of the team. The underlying principles of this work are to do with person centred design, that basically follow those developed in approaches like the Buurtzorg organisation in The Netherlands. The development of the team was in the direction of becoming a self managed team.
The Plan was agreed with the client - but they already had experience of this type of approach, and they know that they could not rely on a fixed outcome - it had to be part of the Understand. But what might be interesting to the reader is that this is really about Transformative change. In this type of change, which is a wicked problem; part of the discovery is to find out where we were going to go. I say we, because this involved transforming peoples thinking as well as the service.
The team - Transforming thinking is something that happens when people decide to explore and accept other possibilities. So, the team that went through this had to be officers from the organisation, plus a manager. They had to undergo the journey, and the only way to do that was for them to actually do it themselves.
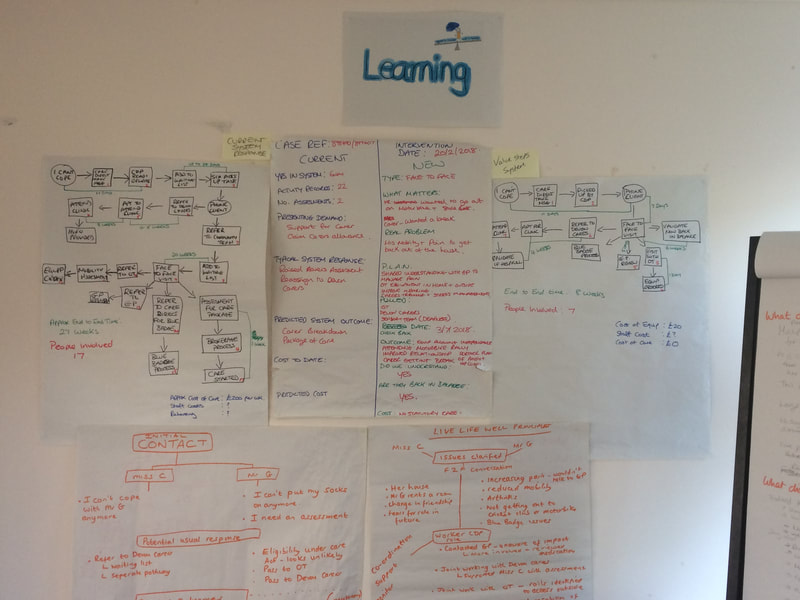
My role as the consultant was as a facilitator, and as a coach. I would give them the right tools at the right time, and they would develop the outcomes. So, no nice clean diagrams from me, they were all generated by the team.
The managers - several managers through the hierarchy were dicretly connected to this work. In particular one manager was increasingly participating. They had to start by being part of the team, and they had to learn. Slowly over time they started to learn new ways of interacting with the team and allowing officers to come up with the solutions. The team manager had to learn how to work with an empowered and self managing team. Whats the role of the manager when the team are self managing?
The Plan was agreed with the client - but they already had experience of this type of approach, and they know that they could not rely on a fixed outcome - it had to be part of the Understand. But what might be interesting to the reader is that this is really about Transformative change. In this type of change, which is a wicked problem; part of the discovery is to find out where we were going to go. I say we, because this involved transforming peoples thinking as well as the service.
The team - Transforming thinking is something that happens when people decide to explore and accept other possibilities. So, the team that went through this had to be officers from the organisation, plus a manager. They had to undergo the journey, and the only way to do that was for them to actually do it themselves.
My role as the consultant was as a facilitator, and as a coach. I would give them the right tools at the right time, and they would develop the outcomes. So, no nice clean diagrams from me, they were all generated by the team.
The managers - several managers through the hierarchy were dicretly connected to this work. In particular one manager was increasingly participating. They had to start by being part of the team, and they had to learn. Slowly over time they started to learn new ways of interacting with the team and allowing officers to come up with the solutions. The team manager had to learn how to work with an empowered and self managing team. Whats the role of the manager when the team are self managing?
The Methodology
Open each section to read more about the methodology used
Understand
Understand is the analysis of the current system, its performance and the impact on the customer. The customer being the person needing help. The approach that was used was to take a team of front line staff and the manager through a series of stages of learning and prototyping - they started by understanding what mattered to the people calling in. They also mapped out all the activities that they took to complete the end to end flow.
Systems thinking - The start of the process has to be to ask why are we here - our purpose? Design thinking - And then we have to understand HOW we achieve this purpose from an outside in perspective. Then we can truly get the customer experience, fully in our mind. In this case we were not able to do this until the prototype stage, this is because this work is so complex, that it was only by trying to design a prototype did we truly understand what mattered to them.
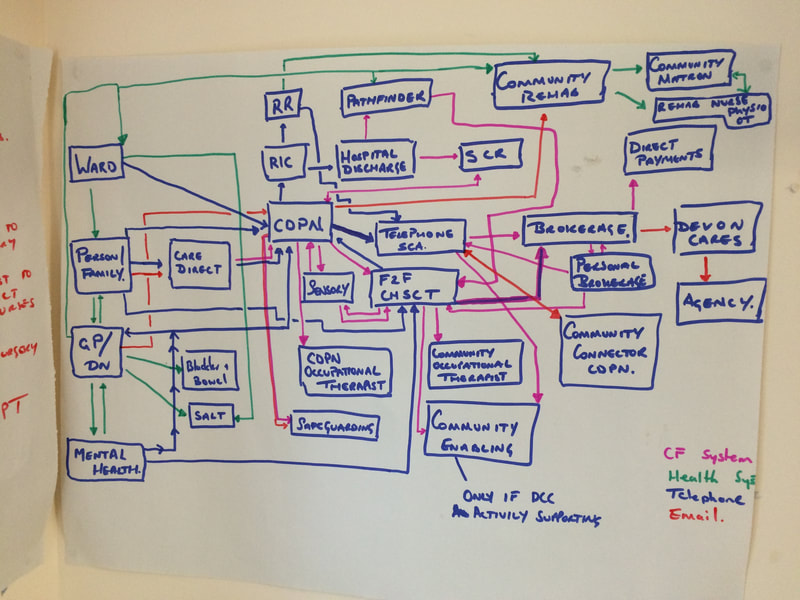
The nature of the demand, its variable nature, and its complexity was very high. The nature of the system under consideration was basically an open system, whose boundaries we had to set far wider than they were used to.
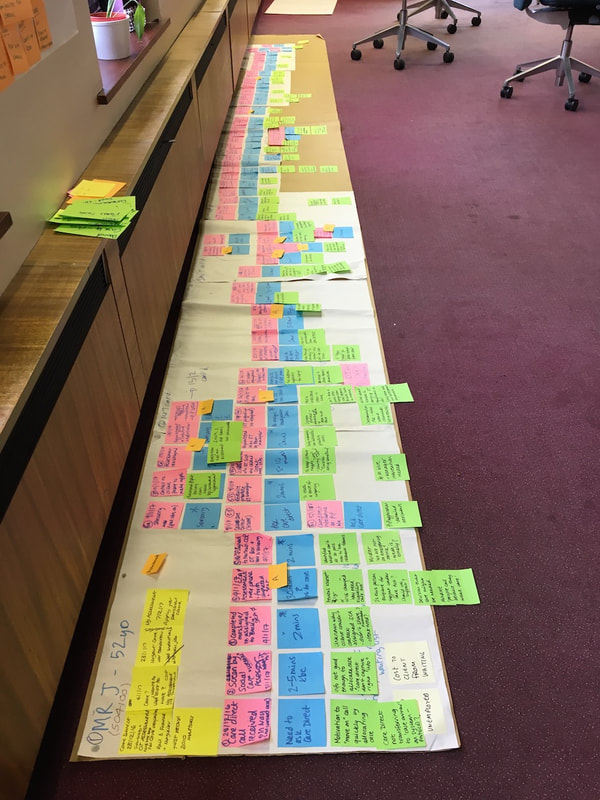
Design thinking - The team spend a few days on developing a workflow map for several examples, that contained each activity. This map is only useful if it tells us something. So, we identified the value and waste. The team were stunned.
Systems thinking - The start of the process has to be to ask why are we here - our purpose? Design thinking - And then we have to understand HOW we achieve this purpose from an outside in perspective. Then we can truly get the customer experience, fully in our mind. In this case we were not able to do this until the prototype stage, this is because this work is so complex, that it was only by trying to design a prototype did we truly understand what mattered to them.
The nature of the demand, its variable nature, and its complexity was very high. The nature of the system under consideration was basically an open system, whose boundaries we had to set far wider than they were used to.
Design thinking - The team spend a few days on developing a workflow map for several examples, that contained each activity. This map is only useful if it tells us something. So, we identified the value and waste. The team were stunned.
Systems thinking - we had to ask ourselves how effective the current system was? The answer was, we didn't know. But we knew that it could work lots better.
experiment & prototype
With a non-transactional workflow, it is not easy to see a new way forward. So, I had to do some work to get the creative juices flowing. These are front line staff that had the old ways of working drummed into them, for years. So...
Design thinking - In the first section of the work, the team worked hard to understand what they could from their expriences and from data. The main place to start was the beginning, which was to Understand the person needing help. Sounds easy, but the team had to go and actually find out.
Background - Staff understand their patients, they do this through assessments.
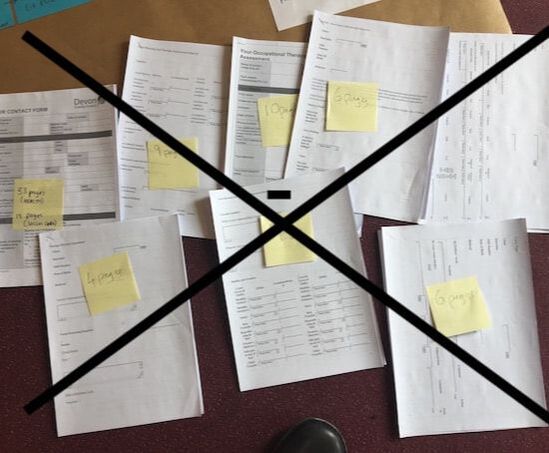
Learning - they learned that by using assessments, this stopped them from them from truly understanding, They learned that Understanding people was really, really difficult! It took several days of coaching and repetition for those team mebers to push aside their current thinking and approaches,a nd learn to listen with no pre-conditions. This variety was key to helping the managers to understand about the nature of variation and standard approaches that restricted that variety.
Systemic design - The team then went on to the next stage, which was to summarise and make sense of what they had understood. But not from a purely medical or professional perspective, but from the perspective of the persona nd those around them.
What we did - we discovered that we had to release our boundaries of our mind, to be able to think of solutions how to help people that they actually needed. Liberate those at the front line to do the right thing.
Learning - that we had to learn completely new ways of listening, evaluating, working collaboratively, and then assisting.
What we did - the team worked through 35 people in ways that were now, and in ways that were defined by the persons needs and circumstances. They had permission to apply new approaches, stop doing things that they did not think they needed, liberating their method and not be restricted by the current operational constraints. The manager ensured that the team were doing the right thing with regard to safety and risk.
Design thinking - In the first section of the work, the team worked hard to understand what they could from their expriences and from data. The main place to start was the beginning, which was to Understand the person needing help. Sounds easy, but the team had to go and actually find out.
Background - Staff understand their patients, they do this through assessments.
Learning - they learned that by using assessments, this stopped them from them from truly understanding, They learned that Understanding people was really, really difficult! It took several days of coaching and repetition for those team mebers to push aside their current thinking and approaches,a nd learn to listen with no pre-conditions. This variety was key to helping the managers to understand about the nature of variation and standard approaches that restricted that variety.
Systemic design - The team then went on to the next stage, which was to summarise and make sense of what they had understood. But not from a purely medical or professional perspective, but from the perspective of the persona nd those around them.
What we did - we discovered that we had to release our boundaries of our mind, to be able to think of solutions how to help people that they actually needed. Liberate those at the front line to do the right thing.
Learning - that we had to learn completely new ways of listening, evaluating, working collaboratively, and then assisting.
What we did - the team worked through 35 people in ways that were now, and in ways that were defined by the persons needs and circumstances. They had permission to apply new approaches, stop doing things that they did not think they needed, liberating their method and not be restricted by the current operational constraints. The manager ensured that the team were doing the right thing with regard to safety and risk.
Human Learning Systems
Human
The main focus of the human aspect covered two main areas. The first was the staff in the team. How they worked together, and also their personal journey of developing a new working culture and relationships with each other. Of significance was psychological safety, the ability to bring their whole selves to work, individual strengths, and trust. The health service is delivered by people, not by technology or other mechanisms. This aspect of staff goes far deeper than simply taking about roles, but more the direction of how people work to their fullest. Dan Pink expresses that a human role should incorporate autonomy in the role, mastery of skills, and purpose with regard to achievement of purpose.
The other side of Human, was the design of a new approach that treated the citizens who needed help as whole people, and not as ‘service users.’ Service users and the focus of citizens in need in the past decades has moved towards people as customers. This means that citizens have to be understood as a totality, often including their relationships with friends and family. This is very different from health based episodic provision.
The main focus of the human aspect covered two main areas. The first was the staff in the team. How they worked together, and also their personal journey of developing a new working culture and relationships with each other. Of significance was psychological safety, the ability to bring their whole selves to work, individual strengths, and trust. The health service is delivered by people, not by technology or other mechanisms. This aspect of staff goes far deeper than simply taking about roles, but more the direction of how people work to their fullest. Dan Pink expresses that a human role should incorporate autonomy in the role, mastery of skills, and purpose with regard to achievement of purpose.
The other side of Human, was the design of a new approach that treated the citizens who needed help as whole people, and not as ‘service users.’ Service users and the focus of citizens in need in the past decades has moved towards people as customers. This means that citizens have to be understood as a totality, often including their relationships with friends and family. This is very different from health based episodic provision.
Learning
The whole purpose of the prototype was to learn what worked and what does not work. It is designed to inform senior leaders, who can then make further informed decisions as to how they would like to take that learning forward. Those leaders themselves need to go through a learning process overt the life of the prototype. The team became adept at summarising the learning experience to a set of activities that occurs in a workshop situation, that takes leaders through journeys of learning. Under no circumstances would any outcomes be written up in the form of reports. And no reports were ever created for this work. Reports simply emphasise the current paradigm, as readers simply use the text to compare their current thinking with what they are reading. In addition, reports fail to convey complex narratives.
The primary mechanism to this progression of the prototype is learning – and learning that is directly experiential. This is required because the current paradigm of how our health services work, is framed in the principles of New Public Management. This design has been in place for so long, that it is very difficult to conceive of new ways of working within that frame. Therefore it is necessary to help leaders to enquire deeply into their mind-sets, to help them to understand a quite different paradigm.
The whole purpose of the prototype was to learn what worked and what does not work. It is designed to inform senior leaders, who can then make further informed decisions as to how they would like to take that learning forward. Those leaders themselves need to go through a learning process overt the life of the prototype. The team became adept at summarising the learning experience to a set of activities that occurs in a workshop situation, that takes leaders through journeys of learning. Under no circumstances would any outcomes be written up in the form of reports. And no reports were ever created for this work. Reports simply emphasise the current paradigm, as readers simply use the text to compare their current thinking with what they are reading. In addition, reports fail to convey complex narratives.
The primary mechanism to this progression of the prototype is learning – and learning that is directly experiential. This is required because the current paradigm of how our health services work, is framed in the principles of New Public Management. This design has been in place for so long, that it is very difficult to conceive of new ways of working within that frame. Therefore it is necessary to help leaders to enquire deeply into their mind-sets, to help them to understand a quite different paradigm.
Systems
The healthcare system is perhaps the complex that is possible to understand. It is both national and encased in legislation. The links that citizens often require cover a myriad of various specialisms and healthcare practice.
The systemic nature of this prototype is in contrast to the mechanistic and reductionist design that currently dominates the health services. This systemic perspective is the frame that the team must embrace, to then focus on the person in need in new ways.
The healthcare system is perhaps the complex that is possible to understand. It is both national and encased in legislation. The links that citizens often require cover a myriad of various specialisms and healthcare practice.
The systemic nature of this prototype is in contrast to the mechanistic and reductionist design that currently dominates the health services. This systemic perspective is the frame that the team must embrace, to then focus on the person in need in new ways.